Understanding Plantar Fasciitis
A sharp sensation in the heel with the first step out of bed. Lingering soreness after standing. Discomfort along the bottom of the foot that comes and goes.
It often continues quietly like this. Stiffness fades as you move, only to return later in the day. At first, it’s easy to ignore. Over time, discomfort can begin to shape how you walk, how long you stand, and which activities you quietly avoid.
These are common early signs of plantar fasciitis, one of the most frequent causes of chronic foot pain.
Plantar fasciitis is often treated as a local foot issue. But lasting relief usually requires a broader view—one that looks at how the entire body moves and adapts. This is where careful assessment and advanced manual therapy can play an important role, helping address not just symptoms, but also locate and correct the underlying patterns contributing to pain.
This is also why simply rubbing tight tissue or focusing only on strengthening the calves rarely leads to lasting change. While those approaches may offer temporary relief, they often miss the bigger picture.
Below, I’ll share what plantar fasciitis actually is, how to recognize it if you—or someone you know—may be experiencing it, and how manual therapy can not only relieve symptoms, but help prevent the pain from returning.
What Is Plantar Fasciitis and Why It Causes Foot Pain
Plantar fasciitis is one of the most common causes of heel pain, a point also reflected in widely used clinical resources such as the Mayo Clinic.
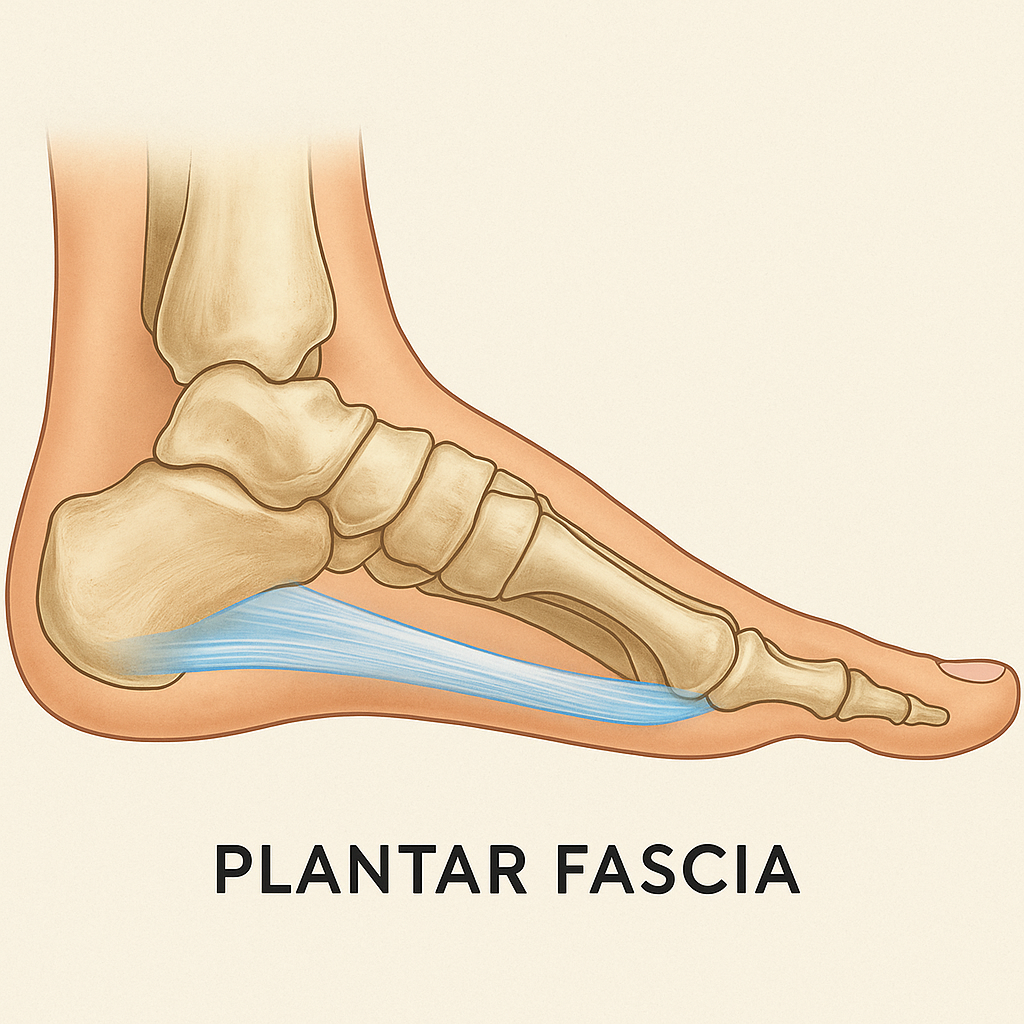
The plantar fascia is a strong band of connective tissue that runs along the bottom of the foot, from the heel toward the toes. Its role is both simple and demanding: to support the arch and help transmit force as you walk, run, and stand.
When this tissue becomes irritated or overloaded, pain often appears near its attachment at the heel. This is why symptoms are commonly felt with the first steps after rest, when the tissue is being asked to adapt quickly after a period of stillness.
Common Signs and Symptoms of Plantar Fasciitis
Plantar fasciitis tends to develop gradually. Common signs include:
- Sharp or aching pain near the heel, especially with the first steps in the morning
- Pain that eases with movement but returns after prolonged standing or activity
- Tenderness along the bottom of the heel or inner arch
- Stiffness in the calves or Achilles tendon
- Discomfort that lingers even as activity levels change
If these symptoms sound familiar, you—or someone you know—may be experiencing plantar fasciitis.
Common Causes of Plantar Fasciitis and Heel Pain
Plantar fasciitis is rarely caused by a single factor. More often, it emerges from a combination of influences that increase strain through the foot over time, such as:
- Repetitive or sustained loading from walking, standing, or athletic activity
- Footwear that doesn’t adequately support or distribute force
- Tightness in the calves or Achilles tendon
- Limited or compromised foot and ankle mobility due to previous injury or altered movement patterns
- Changes in activity level or body weight
- Compromised strength of the hamstrings, glutes, and/or toe muscles
Together, these factors can shift how force travels through the body, asking the plantar fascia to absorb more load than it’s designed to handle.
How Muscle Activation Affects Plantar Fasciitis
Strength or weakness alone doesn’t tell the full story. How muscles coordinate and activate often plays the central role.
When the hamstrings, glutes, or deep foot muscles aren’t contributing effectively, other tissues step in to compensate. Over time, the plantar fascia may be asked to take on excess demand without the support it needs to work efficiently, leading to irritation and pain.
In this way, plantar fasciitis is not just about tissue damage, but about movement patterns that are no longer working efficiently.
How Manual Therapy Helps Relieve Plantar Fasciitis
While rest, ice, and stretching can be helpful as part of treatment, on their own they often fall short of addressing the underlying contributors to plantar fasciitis.
Through manual therapy, I assess the body as a whole—not just the site of pain—and then work to:
- Release unnecessary tension in the plantar fascia and surrounding tissues
- Improve mobility in the ankle, calf, and Achilles tendon
- Support balanced strength and healthy muscle activation patterns
- Restore more efficient movement so the plantar fascia is no longer overloaded
Through this work, I help release tension, restore mobility and efficient movement, and create lasting change—so you can get back to the activities you enjoy, without pain.
A Final Note on Individual Differences
Every body is a little different. Even with common conditions like plantar fasciitis, symptoms don’t always follow a textbook pattern. Foot and heel pain can show up in different ways depending on movement history, activity level, past injuries, and how the body has adapted over time.
If your foot or heel pain doesn’t quite match the signs or symptoms described here, you may not have classic plantar fasciitis, but something related or contributing to similar discomfort. If you’re unsure what’s going on, I’d be happy to help you sort through it. Even if we determine that manual therapy isn’t the right next step, I can help you better understand what’s happening in your body and point you toward the most appropriate course of action.
📍 To learn more or schedule an appointment, visit – www.SantaRosaAdvancedManualTherapy.com